Cataract operation decision making tool
...........how to use it Oct 2004, D Kinshuck
|
When to use it
- This aid is in development.
- It may be helpful to use this for some consultations, particularly
in patients where it is difficult to make a decision.
- The tool may be more useful to the doctor...remind him how to explain
the decision making process to the patient (this will only be necessary
in the minority of consultations).
- Decision making tools may be useful (see),
but naturally this depends on how they are used.
- Naturally very experienced surgeons have lower risks, especially
in 'high risk' patients. Similarly, less experienced surgeons have
higher risks.
- This tool is really designed to give patients an idea as to how
decisions are made, it cannot be very accurate.
- It may be particularly helpful if a patient is hoping for a better
result than the surgeon expects.
- A patient happy with their level of vision is less likely to want
surgery. If a patient is coping well and happy despite their cataracts,
then surgery is not usually needed.
- Eg: An 80y patient with heart disease who drives, with glare at
night and wants to drive at night but who still has good reading
vision, with 6/9 surgery, may want surgery. But if that patient has
risk factors, as below, such as being on anticoagulants, he may be
best without surgery for the time being.
- Many patients believe they will not need to wear spectacles after
cataract surgery, and hence ask for surgery even if their cataract
is in its early stages: if patients want good sight then spectacles
are usually needed. High expectations can lead to unhappy patients.
- Take into account the best achievable visual acuity. For example,
if the patient's sight is very poor, due to cataract AND a condition
such as macular disease, then operate only if the risks are low.
|
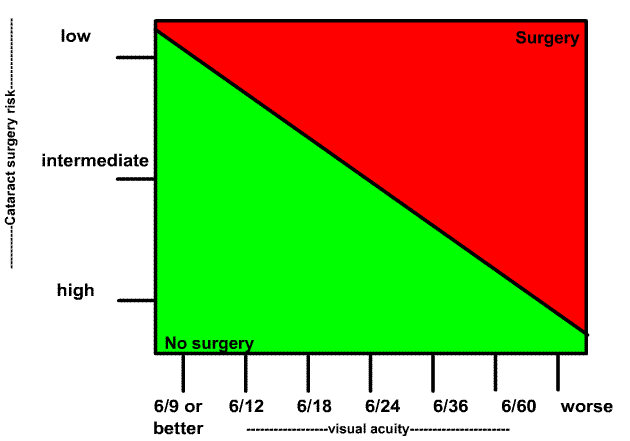
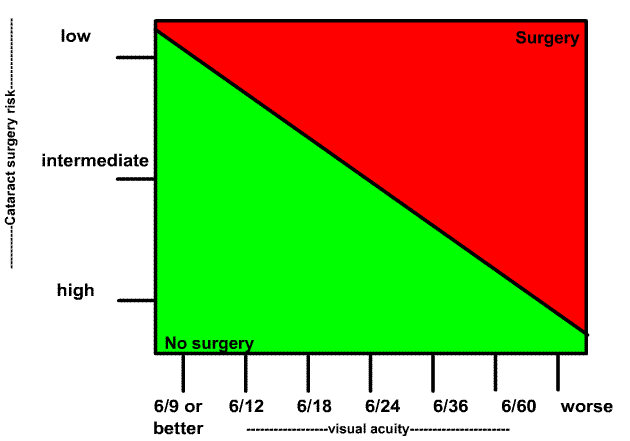
How to use it |
- Use your mouse and move it over the risk slider (a blue blob), and
move it to the appropriate risk (vertical, y, axis).
- Do the same with the horizontal visual acuity slider (another blue
blob), and line it up to the 'appropriate' visual acuity for that patient
(the x axis) (Visual acuity in the eye being considered for surgery).
- If the target circle is on red, surgery may be best, if on green, no
surgery at this stage may be best.
- Use the tool with the patient watching on your desktop PC monitor.
Alternatively, print this page and use the static image at the bottom,
marking the lines with a pen with the patient present.
|
with some ideas from Muhtaseb's & Mahmood study. |
| Low risk related |
- good general health
- no eye risk factors/pathology
- aware of small risk of problems
- may need spectacles after surgery (needs to be aware of this)
- must be able to lie comfortably for time of surgery
- Blood pressure less than 140 systolic
|
| Reasonably low risk |
- reasonable general health
- mild eye problems, such as controlled glaucoma
- controlled diabetes & no retinopathy
- professionals see
|
Intermediate risk
|
one point in Muhtaseb's study
- Previous vitrectomy
- Corneal scarring
- Small pupil (<3mm)
- Shallow anterior chamber (<2.5mm)
- age >88years
- high ametropia: >6d myopia or hypermetropia
- posterior capsule plaque
- poor eye position (e.g. enophthalmos, narrow palpebral fissure)
- tremor
- communication difficulties
- breathing difficulties
- using flomax
any time in the last 2 years If the pupil dilates fully pre-operatively,
the risk is lower. If the pupil does not dilate, expect iris prolapse
during surgery (flomax=tamulosin).
...and Good Hope adds
- mild fuchs dystrophy
- other risks
- emphysema
- background diabetic retinopathy (may develop maculopathy)
- previous trabeculectomy and controlled pressure and dilated pupil
(slightly greater risk if pupil small/experienced surgeon)
- difficult lying still for 10-40 minutes
- anticoagulants
- Blood pressure higher than 140 systolic...increases risk of cystoid
macular oedema etc
- obesity...shallow AC
|
| High risk |
- incomplete pupil dilation (59.5% vs 8.8%) Mahmood
- Dense/total/white or brunescent cataract..use
procedures such as vision blue
- Pseudoexfoliation (5.6% vs 1.4%) Mahmood
- phacodonesis
- severe dry eyes
- a combination of the above risk factors
- previous vitrectomy (7.8% vs 2.2%) Mahmood
- related to surgical experience, topical (14.3% vs 3.1%) and sub-Tenon's
(51.4% vs 37.2%) anaesthesia Mahmood
- requirement for vision blue (trypan blue ophthalmic solution) (13.7%
vs 2.4%). Mahmood
..and Good Hope adds
- severe breathing difficulties or very poor health
- posterior
polar cataract..may need vitrectomy
- severe fuchs dystrophy
- poor general health
- uncontrolled glaucoma
- diabetic maculopathy/retinopathy
(if active, this gets worse after surgery)
- emphysema on oxygen therapy at home
- advanced glaucoma with very little visual field remaining.
- active
blepharitis
- severe atopic conjuncitivitis as below
- extreme obesity
|
Shallow AC/hypermetropia
after lecture given 2005 |
- expect problems if AC <2mm and lens thickness >5mm
- high risk axial length (AL) <20mm...
nanophthalmos
- use AC maintainer 20-22 mm
- vitrectomy first for highest risk <20mm, especially if lens thickness/axial
length ratio >20%, and AC maintainer for cataract surgery: large PI
with vitrector probe at end
- use Hoffer Q formula
|
| Blepharitis |
at time of listing
- treat blepharitis with lid hygiene
- severe cases need systemic oxytetracycline/doxycyline if tolerated
- use chloramphenicol (or alternative drops) to clear blepharitis
- active blepharitis..AVOID SURGERY if possible
- check repsonse 2 weeks before surgery
week pre-operatively
- start intensive chloramphenicol drops 3-7 days prior to surgery
(or alternative drops)
- check for active blepharitis
pre-operatively
- use polvidone
iodine to clean eye, and leave it to clean for several minutes
before local anaesthetic
- repeat before sstarting surgery
post-operatively, if lid not completely clean
- check patient frist day and 2-3 days later
- warn patient to attend as an emergency if the eye becomes achy,
painful, with decreasing vision
|
| Severe dry eyes/conjunctival
disease |
- Avoid 'Maxitrol' drops after cataract surgery if you have dry eyes
or conjunctival disease. It can cause very severe corneal problems (Midland
Ophth Meeting, 2005).
- Preservative free drops for severe cases
- Maxidex AND chloramphenical (with preservatives, in combination, as
separate drops) are well tolerated in mildly dry eyes.
- Use a schirmers tears test prior to cataract surgery if the patient's
history suggests dry eyes. Also, if the patient has significant rheumatoid
arthritis.
- Use lacrimal plugs...normally we insert these AFTER the operation,
perhaps at the first post-op visit.
|
| Inflamatory uveitis & Fuchs
Heterochromic Cyclitis (FHC) |
- Usually increase steroids 4-8 weeks before surgery
- pre-operatively boost steroids with a pulse
- FHC patients certainly benefit from pulsed methylprednisolone just
before surgery, and have much higher risk of problems
- Non-steroidal
anti-inflammatory NSAID drops help to prevent post-op macular
oedema. They are not yet given routinely because of the expense. Even
starting 2 days pre-operatively can be helpful.NSAID after cataract
surgery are just as effective (but more expensive).
- Steroids or NSAID should be given 2 weeks pre-operatively in uveitis
patients... uveitis experts often have local guidelines.
|
| Severe eczema |
- cataracts are a common complication
- atopes...develop anterior cortical cataracts... surgery is difficult
needs vision blue; rhexis turns out; cortex leaks out; young patients
especially atopes have double risk; zonules weak; fibrosed lids-shallow
fornix..cicatricial changes increase risks further;
- postop...capsule phimosis; hole in post cap...more likely to detach
retina
- sodium Hyaluronate drops (vismed); hyalocomod; help lubricate after
surgery
|