Glaucoma for professionals David Kinshuck |
|
|
|
Cyclodiode laser for rubeotic glaucoma |
|
Some notes
|
 |
|
5 FU |
|
Some notes
|
|
OCT etc |
|
Brittle angles |
typical case, intermittent IOP rises initially, then constant....eg congenital glaucoma, ectropian uvea, axenfeld/reigers, high iris insertion, JOAG, trauma, previous angle closure, plateau iris, uveitis, PXF, HZO, HSVU, high myope, steroid, very old patient. |
After refractive surgery |
|
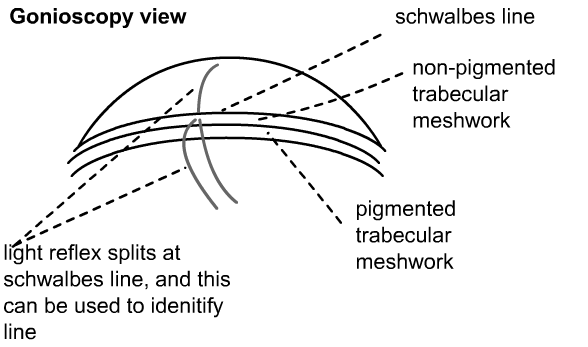
How to find schwalbe's line etc |
 |
NA-AION & NA-PION |
|
Is visual field loss from glaucoma or toxic optic neuropathy |
|
Glaucoma or progressive optic nerve lesion? |
|
|
Glaucoma and night (notes from College, 2007) |
|
|
Glaucoma and steroids (notes from College, 2007) |
|
|
Glaucoma / cupped discs (notes from College, 2007) |
|
|
Glaucoma and arcuate scotomas (notes from College, 2007) |
|
|
Glaucoma and optic disc drusen (notes from College, 2007) |
|
|
Glaucoma notch (notes from College, 2007) |
|
Asymmetric glaucoma |
| Suspect carotid artery stenosis |
More about pressures and anticardiolipin antibody (includes notes from College, 2008) |
|
Blood pressure & ocular perfusion, |
Blood pressure may have a role in glaucoma. Some papers indicate that too low a blood pressure may be harmful, whilst others suggest that a reasonably low blood pressure might help. It is likely that the ocular blood flow (i.e. the blood flow into the optic nerve) is likely to be the most important factor (Costa 09, Liang 08)
|
Symptoms (notes from College, 2008) |
|
Examining Fields (2008) |
|
Field changes fluctuate BJO 2011 |
Measure discs (2008) |
|
types of cupping
|
Notes about fields/disc haemorrhages (2008) |
|
Glaucoma genes |
|
Poor compliance |
See Lacey J, Cate H, Broadway DC 2009
|
Chronic conjunctivitis |
We are all familiar with a true allergy (eczema around the eyes, itchy eyes), but many patients develop more chronic changes.
|
allergic conjunctivitis: lots of papillae |
SLT laser |
SLT lowers pressure Singh09
|
|
| The address of this site ('org' changing to 'nhs') is changing from http://www.goodhope.org.uk/departments/eyedept/ to http://www.goodhope.nhs.uk/departments/eyedept/ |
|