Age Related Macular Degeneration (ARMD) pathology & treatment David Kinshuck & Monique Hope-Ross |
| This is a very long page..see separate pages This page.................................................................
Distortion
of vision and other symptoms:
'Wet' or neovascular types of ARMD
Further details
|
|
ARMD introduction |
ARMD is usually a progressive condition, affecting the center of the retina and the centre of the vision. Invisible early changes occur, then usually some type of dry ARMD, such as drusen or geographic atrophy. Later, the dry changes may progress, usually slowly, to cause more atrophy and damage to the central retina. The dry changes are bascially aging, wearing out of the central retina. Then in some people, wet changes develop, with blood vessel growth and leakage in the macular area. These wet changes can be slowed down with anti-VEGF drugs (see this page or wet ARMD page). Age-related macular degeneration is explained in more detail on other web-sites, such as the RNIB and NIH. This is an excellent animation: www.eyesight.org. This page summarises our current knowledge. |
Contributing factors: aging, genes, diet, smoking, etc |
Age-related macular degeneration (ARMD) is one of the commonest causes of poor sight in developed countries. Whilst the causes are different in different people, certain factors may contribute. The main factor is age. |
| age | age is the main factor |
| summary | |
| smoking | contributes 32% overall, even passive smoking |
| diet | related up to ~30%; a high cholesterol from an unhealthy diet or genes Klein (2010); Toothbrushing helps. (tooth decay promotes conditions such as rheumatoid arthiritis) |
| blood pressure | high blood pressure damages the circulation...2010 target is 140 systolic
in clinic, 10 lower for diabetes. 10 lower at home. That is 120 at home
for diabetes. Best below 120 2 medications often required. |
| exercise | via blood pressure effects; regular exercise reduces risk by 70% |
| genes | ~50% is directly due to the genes we inherit, see and Gene page |
|
a high fat diet 10% (2010) |
|
| exercise | reduces progression to neovascular ARMD by 70% |
| airbourne pollution | This has been found to cause cardiovascular disease, and therefore is likely to contribute to macular disease. In urban environments, ~8% of deaths are generally attributed to pollution. More definitive proof is awaited, but may take years to obtain, especially the contribution of pollution to ARMD specifically. |
Excess alcohol is also related to ARMD, see |
|
| sunlight | Sunlight exposure, especially the summer sun, contributes to ARMD; and sunglasses protect, see. Some sunlight exposure is important...gentle sun exposure increases vitamin D production, and this will reduce the risk of many conditions such as diabetes, osteoporosis, and prostate cancer. |
| other | Other pro-inflammatory states can influence the condition, such as chlamydia High CRP, Ophthalmology 2010 |
| macular pigment | ARMD is much commoner in Caucasians...the lighter the skin or the least retinal macular pigment is related to risk. ARMD is unusual in Afro-Caribbeans, and this may be because the 'elastin' layer is thicker. Especially in wet ARMD with CNV, the elastin layer acts as a barrier to the growing CNV (new vessels). Elastin is part of Bruchs membrane link |
Other countries |
Some communities in Japan did not develop macular degeneration as people aged, but as soon as they started eating Western food the condition started to occur. Similarly, when Japanese people move to Western countries, they develop the condition more frequently. These observations suggest that the high fat (and type of fats, such as saturated and trans-fats) in our diet, the lack of protective fats (omega 3s, from fish), and salt (by increasing blood pressure) increases the number of people with ARMD. Lack of exercise as we drive everywhere in Western countries will contribute. |
|
Genes |
We inherit these from our parents. Genes are the genetic information that tells our body what chemicals to make. Overall, our genes may contribute to more than 50% of ARMD. We will soon be able to work out who is at risk...the main genes have been found. Tsee See Gene page The genes that may cause macular degeneration probably control the way used-up chemicals are removed from the eye. Being long-sighted (hyperopic) is also a risk factor |
A healthy lifestyle |
A healthy lifestyle helps to prevent
age related macular degeneration. This is important for the younger relations
of age related macular degeneration sufferers:
|
Smoking |
|
|
Blood Pressure & Exercise |
|
|
Alcohol |
| Too much may contribute indirectly by increasing blood pressure, and is related to ARMD, see. Red wine may be healthier in small amounts). Blood pressure rises after drinking (opposite...drinking 4 pints/bottle of wine). Each gram of alcohol puts systolic blood pressure up 0.24mmmHg, diastolic 0.16 mmHg. This means 1 pint of beer (2 units, each unit 8g alcohol) with 16gm of alcohol, drunk every day, will put the systolic blood pressure up (16 x 0.25=) 4mmHg. |
enlarge |
Diet |
Experts recommend a healthy diet.
Fruit/vegetables prevent 36-50% of ARMD see, see and see (fruit & vegetables lower homocysteine levels, and this improves blood flow). Pulses like beans are fine. Bread, pasta, rice and potatoes provide ‘energy’. Vegetarians have lower blood pressures and healthier lipid levels, see . A healthy diet reduces homocysteine levels, which are associated with ARMD . Certainly saturated fats increase the risk of ARMD; and fish and polyunsaturated fats halve the risk. Avoiding certain fats helps, with strong evidence here (explained more clearly here for heart disease). Nuts may help prevent ARMD (small amounts...they are fattening). |
5-9 portions of fruit/vegetables
a day, with portions of different colours The Guardian (2005) reviewed healthy diets etc, here, here , here , here and so on. See some epidemiology |
Vitamin supplements |
As the macula is the most metabolically active area in the body, with the greatest oxygen demand, it has been thought that antioxidants such as vitamins may play a critical role. The retina contains the pigments carotenoids lutein, xeaxanthin, mesoxanthin. Lutein is in darg green leaves such as kale and spinach, and most of us do not eat enough. Xeaxanthin is in orange peppers, corn, nectarines and oranges (and other yellow/orange fruits/vegetable). 'Higher dietary intake of lutein/zeaxanthin was independently associated with decreased likelihood of having neovascular AMD, geographic atrophy, and large or extensive intermediate drusen' Seddon. These vitamins are in the 'AREDS2' supplements Lack of vitamins has been linked to macular degeneration If you are unable to eat this many vegetables, AREDS2 supplements may help, but too many vitamins may be harmful. |
The AREDS1 vitamins reduce ARMD by 25%. It is not known whether or not they help patients who have a healthy diet. |
ICap (Alcon), is available in pharmacies and optometrists. This
has lutein and other vitamins in, and had been recommended by some
ophthalmologists. Beta-carotene supplements are not recommended
for smokers, as they may contribute to lung cancer. I Cap is similar
to the AREDS
vitamins that reduced ARMD risk by 28%.
zeoxanthin , Against., BMJ |
Oily fish |
| Oily fish twice a week reduces ARMD by 40%, especially oily fish such as tuna, mackerel, sardines, herring, and salmon. A Japanese diet may be helpful as above. Other omega 3 fats are helpful. See |
Cholesterol & statins |
ARMD is commoner in people with higher cholesterol levels. Atherosclerosis, caused by a high cholesterol, does contribute to ARMD, see Statin treatment reduces macular degeneration. See see,
Although statin tablets are not yet formally recommended by
all agencies, this author would recommend them for people with ARMD. Naturally all relatives of ARMD patients should address this issue of fat levels in the blood, sticking to a low fat diet with plenty of exercise, avoiding obesity, just as described on this page for ARMD patients. |
Cataract surgery |
| One paper suggests cataract surgery leads to an extra 4-5 times risk of developing neovascular macular changes or dry ARMD. Another states this is not so AREDS 25. Certainly patients with early ARMD undergoing cataract surgery should be warned of symptoms, that is distortion or changes in central vision, and attention should be sought in a few days. Also. |
|
Vitreous changes |
| If the vitreous is separated from the macular the risk of CNV is significantly reduced AMJO 09. This is a new observation. |
|
|
The pathology of ARMD (Age-related macular degeneration) |
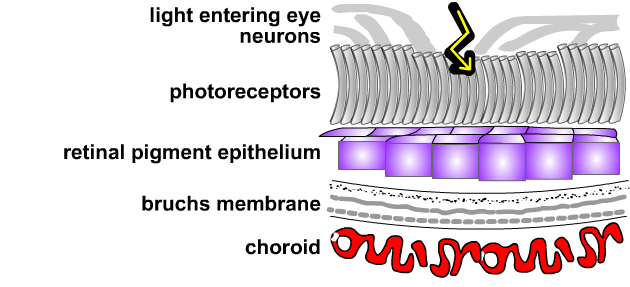
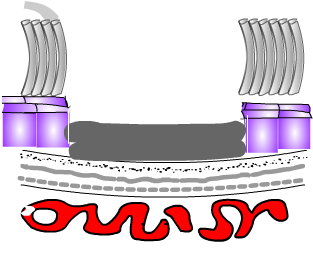
Dry ARMD progresses over many years (this page). In some types of dry ARMD progression may be very slow, but it may be quicker in other types. Sight does deteriorate, but most people manage to cope well, although reading is difficult and life may be different. Dry ARMD may progress to the 'wet type', but this is not always the case. Wet ARMD begins as new vessels growth in the macular area, causing retinal leakage and swelling. Seepage. It progresses to cause a scar in the macular area. If the scar is small, sight is reasonable; if large, the sight can be very poor. Imagine your retina has five layers. Normally this retinal appearance stays constant even in old age, but changes may develop as you get older. |
|
Invisible changes |
|
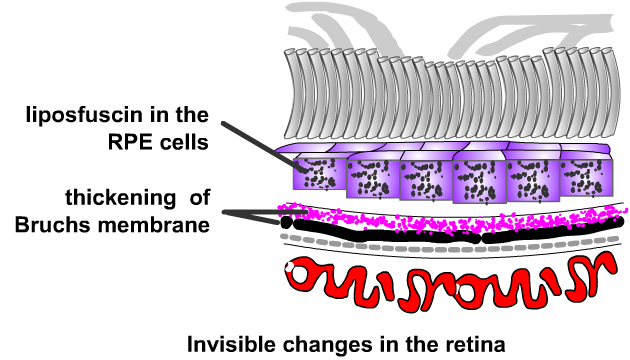
As we get older, changes develop in the retina. The bruchs membrane thickens and the choroidal blood vessels change. see diagram The thickened bruchs membrane prevents waste products leaving the retina (see animation and the link), and also prevents nutrients entering. This is thought to be a direct cause of the condition. Lipofuscin (type of fat) accumulates in the retinal pigment epithelium; this damages the pigment cells which eventually die. The choroidal circulation changes...the blood vessels become larger but fewer. This is probably mainly due to a 'hardening of the arteries' that happens elsewhere in the body, particularly with a Western diet. The invisible changes progress to cause dry ARMD,
These changes are described with photos below. |
|
What does a person notice with these early changes ? |
If you notice these problems then you are probably at risk and need a check from an optometrist or ophthalmologist. If there are no visible changes, the author would strongly recommend a healthy lifestyle as prevention...it helps your general health in any respect. (This section: after Prof. Bird). |
Types of 'dry' macular degeneration |
|
Progression of 'Dry' macular degeneration |
Once the invisible changes above develop, the dry changes develop.
|
The retina becomes very thin, just as though it is worn out. The patches of such thin retina do not 'see', so the central vision becomes patchy. Essentially it is a type of wear and tear. |
|
Dry types of macular degeneration can get very slowly worse, but only affect the macular area. The rest of the retina, which helps you see at the sides so you can walk round the house, always stays good. The progression is a usually a very slow process taking years. This movie is excellent. If this wear and tear is mild you may be able to read and even drive,
although it takes a little longer to adjust to different lighting. Some types are
non progressive, and not discussed here in detail (such as old macular
holes). The appearance of the retina may be same in different patients (phenotype.)
But in fact each person's condition (even though it looks the same
to the doctor on the photographs or scans may have different factors such
as different genes (genotype).
|
Patchy vision in atrophic macular degeneration
|
Drusen |
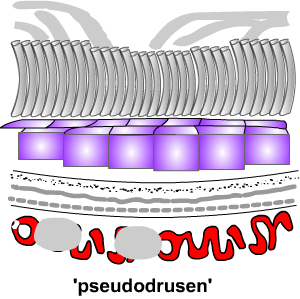
There are different types of drusen. They are one of the signs of dry ARMD, and soft and pseudodrusen/reticular predisposed to wet ARMD.. |
|
Hard drusen: If they are well defined
with a sharp edge, the sight is likely to stay good. Soft drusen: If they are a little like cotton wool, they are more serious as they may lead to more serious disease with 'exudative changes' as below: prevention is most important (see above). Reference. |
and another large one. another See hard drusen (right) & case.
|
enlarge...white arrow is pointing to one of the large soft drusens
|
Drusen look like little white spots in the retina. See tiny drusen. These are accumulations of material, probably some waste products of the retinal cells. These are common, and do not usually affect the sight. The accumulation occurs as bruch's membrane becomes thicker and prevents the free flow of materials to and from the light or photoreceptors layer. Also, the retinal pigment cells accumulate lipofuscin. This pigment will also slow down the passage of chemicals to and from the retina. People with a lot of drusen in the central retina have slightly reduced sight. If there are a few drusen you may be said to have very early 'dry' macular degeneration.
|
|
|
Drusen are slightly related to cholesterol levels. It is logical that reducing the cholesterol will slow down drusen development and therefore slow macular degeneration.Drusen are linked to choroidal blood flow reductions Retina11 UK cholesterol target is 4.5mmol/l, and the World
Health Organisation recommends less than 3.5 as ideal, although risks
increase above 2.5.
|
Pseudodrusen / reticular drusen Reticular drusen/ pseudodrusen are vascular changes in the choroid, which appear as RPE changes on the OCT. However, this is an artefact...the changes are in the choroid risk. Such drusen may lead to wet ARMD: they are related to chromosome 10 gene differences, See Photo Autofluoresence is helpful. See types of drusen, risks and epidemiology. Soft drusen are inherited: see CFH Y402H. Drusen come and go BJ0 2010 Types of drusen with photos BJO 2011.Basal laminar drusen OCT 2010 |
 |
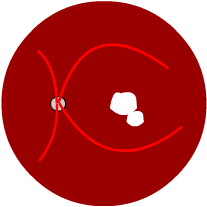
Geographic atrophy (GA) |
|
Areas of thin retina develop, like the patterns of countries of the world. The areas get bigger over years, slowly causing more damage to the sight. Geographic atrophy is the main type of dry ARMD. See a photo Geographic atrophy (GA) accounts for a third of ARMD, with new 12,000 cases a year in the UK. It is believed to be caused by retinal pigment epithelial atrophy leading to cell death. It is best examined with the autofluorescence technique but this is seldom available Retina 2010. There is no treatment available yet, although trials are in place. FAF photo. Atrophic myopic macular degeneration is usually similar. We now know here that the risk of passive smoking (doubles the risk) and personal smoking (triples the risk) of both geographic atrophy. See genes and here. |
 |
It is now clear that GA can lead to wet ARMD, particularly if the GA has an irregular outline ('lobulated'). There is a gene contribution from chromosome 10 genes. This is a more rapidly progressing form, with basal laminar deposits. So GA is not one disease...it is the end stage of many different types of 'dry' ARMD, and an intermediate type in others. It is still not known whether the primary priblem is in the retinal pigment epithelium, choroid, or photoreceptors. GA affects 1/3 people >75y. |
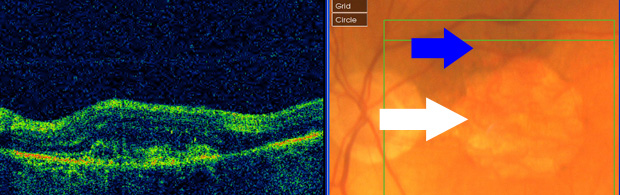 |
enlarge...white arrow is pointing to the geographic change. This progressed over 7 years. Just recently, sight deteroirated, and there are cnv (wet ARMD) which has just begun (blue arrow). Patient male, born 1932. (Only 7% of GA leads to cnv). |
Autofluorescence can be used to predict the progression rate. |
Mixed |
Changes may include thinning of the retina, drusen, pigmentation, or thickening of the retina. There is a variable outcome. ‘Prevention’ may help.
|
 |
Adult onset foveomacular vitelliform dystrophy (AOFVD) |
This is a type of dry macular degeneration (ARMD). The damage is confined to the centre of the macula, the fovea. This is a very small central area, and has been described by Gass, and here. Generally the prognosis is good. However, the retina does become thin in the
affected area, and the sight may get slightly worse with age. See
|
The
centre of the retina (the fovea) is affected, |
|
Distortion
of vision and other symptoms:
|
|
How would you know if you have the 'neovascular' type of age related macular degeneration? Some symptoms suggest you may be developing the problem
If you do develop distortion of vision you usually need to see your ophthalmologist or have ascan at your optometrists within a few days.In the UK you may need to discuss this with your GP, or in a large city attend the Eye Emergency department. See the amsler test below. Your ophthalmologist will recommend an OCT scan, and this shows the wet ARMD immediately. In addition may recommend tests such as a fluorescein angiogram. The angiogram tells the doctor if there are new vessels, where they are, what type they are, and what type of treatment if needed. Wet ARMD progresses 4 times faster (a 400% increase in progression
rate) in smokers.
Dry ARMD may develop into 'wet' ARMD (4%/year). |
Amsler grid test |
Patients should be given the Amsler Grid test to use every day, or at least once a week, at home. These authors recommend this test, although personally I have found that patients may still present late (this is a major problem). Patients are given a grid, told to look at the central spot with their reading glassses on, using one eye at a time. If any of the adjacent lines become bent or wiggly or distorted, then CNV (blood vessels growing under the macula) may be present, and patients should see their ophthalmologist (in Birmingham attend the Eye Centre Casualty, City Hospital). The test is explained well here . A home device enabling early detection of wet ARMD Retina 2010. Unfortunately visual changes follow changes that can be detected by OCT scans BJO 2011 CNV are detected
as compared with OCT. Monthly OCTs are necessary to detect recurrences! |
Distortion of straight lines which may start to appear crooked over a few weeks usually means the ARMD is progressing. Sometimes this is due to the 'neovascular' ARMD developing, and you are advised to be checked in case laser may help. |
ARMD and the other eye |
Unfortunately age related macular degeneration can affect the other eye. See healthy lifestyle above: this may help. If you do notice a change in your sight, see distortion above. See a search . Risk from drusen. The atrophic or dry type usually does occur in both eyes, but remember this generally gets very slowly.There may be a gap of years before the wet ARMD develops in the second eye. |
|
Wet ARMD (exudative/leaky) |
There are different types of wet ARMD
In wet ARMD the damaged retina releases a chemical VEGF (Vascular endothelial growth factor). The VEGF stimulates blood vessel growth, to produce the different types of wet ARMD. In addition, the new blood vessels leak, causing fluid under the retina in these condtions. |
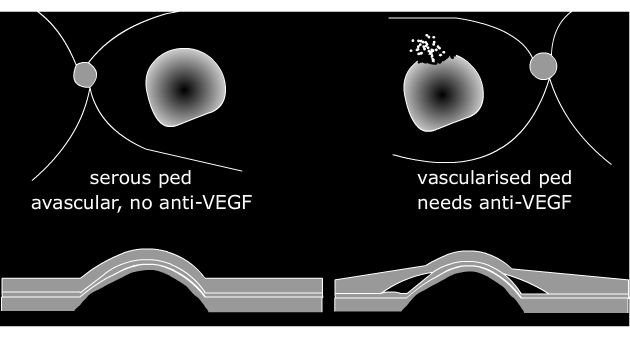
Vascularised retinal pigment epithelial detachment (PED): Occult CNV type 1 |
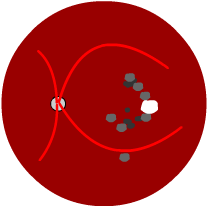
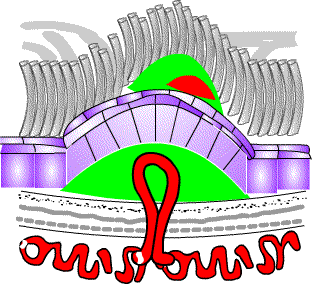
In a few people, the dry macular degeneration turns into this type of ARMD. Occasionally, there may have been no obvious 'dry' changes visible before this develops. In this type the damaged area looks like a dome. Fluid leaks under the retina, hence the term 'wet'. Anti-VEGF drugs are used, although is not always effective. Occasionally these drugs can cause the retina to 'rip', causing more loss of sight Eye 2011. Overall, 15% of PEDs rip, but the risk is proportional to the PED size, so a large PED is much more likely to rip. The rip typically occurs 2 months after starting Lucentis.The rip may not cause that much visual loss initially, but central vision may get worse over time. The PED will not reduce in size with treatment, but treatment will reduce intraretinal and subretinal fluid. Retina 2011 Generally ARMD with a PED is classified as 'occult' CNV, type 1. Outcomes Eye 11 Avascular PEDThere is another type of PED without any vascular element. In younger patients this is usually part of Central Serous Retinopathy. In older patients this is usually part of ARMD, and is classified as an avascular or serous ped: anti-growth factor treatment is not helpful (Eye 2010). However, if the other eye has had wet ARMD, then such as eye is at very high risk of wet ARMD itself. Eye 2012 Really (I suggest) that such eye should have regular OCT examinations, perhaps every 3 months: as yet there is no evidence to prove that this will help, but logically it will help by detecting very early disease that is much easier to treat. |
See a case. There are 3 types of PED, reviewed here (avascular, occult, polypoidal).
|
 |
||
| there is a 'PED' only, no leak | enlarge | 'PED', with a leak under the retina (shown here) or in the retina |
‘Occult’ CNV type 2 (no 'PED') |
In this type of ARMD, there are new blood vessels, but they are not clearly seen with the angiogram. ‘Occult’ CNV is the term given to a specific ‘blotchy’ appearance of the angiogram. Occult ARMD is probably an early phase of classic, see . Occult and classic patterns can occur together. Anti-VEGF drugs are used and results are generally good. The symptoms of this type of CNV are the same as 'classic CNV' . Without teatment, this type 2 occult CNV usually turns into classic CNV over the next months or years, to cause poor central vision. Large occult membranes can develop haemorrhages with anti-VEGF treatment (BJO 2008). |
|
Classic neovascular ARMD (also called ‘classic CNV’) |
|
Some dry types of macular degeneration progress to form this type of wet ARMD. It is very difficult to predict whose dry ARMD will progress, but the risk factors include those mentioned above (soft drusen, high blood pressure, smoking, poor diet, lack of exercise). When blood vessels grow under the macula, this is termed choroidal neovascularisation (CNV or CCNV). When the new vessels are seen easily on a fluorescein angiogram, they are called 'classic CNV': They look like a net of blood vessels. When a doctor looks in the retina looks elevated, there may be tiny haemorrhages, a grey area, or exudaes. This photo is a severe case. In milder cases vision may still be good. The condition may develop over days or weeks, with increasing distortion or blurred central vision. If this process is mild you can still read, but if it becomes severe reading with any magnifier is impossible. Treatment, if possible, includes the anti_VEGF drugs Avastin & Lucentis. Laser PDT may help in addition. If you notice the symptoms (central vision becoming distorted or blurred, sometimes like looking through water) you should have your eye checked with an OCT scan: see distortion.. This is usually a very serious type of macular degeneration, serious because it can cause very poor sight. It never blinds in the sense that you cannot see light and dark, but in its serious form it can damage the central vision so you can only see fingers or even the movements of hands. Once again, the side vision will normally be good, so you should always be able to walk around the house. The CNV grow at 20�/day, reaching 3000 � in 6 months.
They can be extremely difficult to see in early stages. Small membranes
gain, on average, 5 lines of vision with the Lucentis. The condition is occasionally unresponsive to treatment. Surgery/other treatment |
New vessels growing under the central retina in a 'classic' pattern: PDT treatment may help
|
|||||||||||||||
Polypoidal choroidal vasculopathy |
The condition is seen as a branching choroidal network of vessels with vascular dilatation. It is more common in Chinese and Afro-Caribbeans. The choridal neovascularisation often occurs with a serous haemorrhagic PED. It is discussed in more detail here. |
|
||||||
Myopic CNV |
In this type of myopic macula disease, new vessels grow in the macula area. 5% of highly myopic eyes (more than -6.00d) develop CNV. This is similar to wet ARMD, but in myopia it may occur in much younger people. However, it is much commoner in older people with myopia. These new vessels are called 'CNV'...choroidal new vessels or choroidal neoovascularisation, as the blood vessels originate in the choroid and grow under the retina. The CNV cause retinal leakage and swelling. The condition progresses to cause a scar in the macular area. If the scar is small, sight is reasonable; if large, the sight can be very poor. The long term prognosis is not good: most eyes develop less than <6/60 vision. Younger patients have a better prognosis..the CNV get walled off. All types of wet ARMD (CNV) will progress 4 times faster in smokers, a 400% increase. In addition to smoking, high blood pressure, poor diet, lack of exercise increase the likelihood of progression and progression rate. |
New vessels growing under the central retina in myopia (similar anatomically to regular CNV) enlarge photo photo Myopic CNV Arevalo , Ruiz-Moreno, Avastin, Chan 2008 Wakabayashi 09 Some CNV are related to newly developed areas of lacquer cracks Eye 2011. |
| See treatment of myopic CNV. |
Extensive submacular haemorrhage due to CNV (choroidal neovasularisation...wet amd) |
Occasionally large haemorrhages develop in the macular area. These are more likely in smokers, aspirin/anticoagulant users, especially if there is hypertension, or in very elderly patients. Various treatments have been tried. |
 |
Extensive submacular haemorrhage: gas tampanade |
Perhaps the best treatment at present is gas tampanade. (Sacu 09). Injection of tissue plaminogen activator followed by gas often displaces the blood. By displacing the blood, vision may imporve, but also there will be less maular scarring and better sight in the long-term.
|
|
|
Laser and anti-VEGF injection treatment |
If the choroidal new vessels (CNV) are not in the very centre of the retina, regular laser can help. (Laser is a very bright light that makes tiny burns at the back of the eye.) This appearance is called classic extra-foveal CNV. This treatment is only suitable if the CNV are well away from the fovea. Laser is not suitable near the fovea, as over the years laser burns expand and this can reduce central vision.
|
If the area of neovascular ARMD (CNV),
shown as the red area, is not under the very centre (the yellow
spot, called the fovea), and laser was used. |
|
Most people with neovascular ARMD have CNV in the centre of the retina. This appearance is called sub-foveal CNV. In general treatment will be with Avastin (or Lucentis) anti-VEGF drugs The drugs are given by injections in the eye itself about 8-12 times a year. Avastin/Lucentis usually cause regression of new vessel growth. But unfortunately, after 4 weeks, the effect of the drugs wears off, and then the new vessels start to grow again, needing repeated treatment. Such injections may be needed every month for years. Early CNV responds best, needing fewer injections. Here is an up to date treatment plan. |
CNV under the fovea |
|
Laser & other treatments for neovascular ARMD |
There are other treatments for neovascular ARMD (CNV), such as surgery, but apart from PDT laser these are not very successful and not in general use: |
|
||||||||||
|
|||||||||||
|
Scarring |
|
Many types of macular degeneration progress to cause scarring. 'Dry' types usually progress more slowly, but occasionally can cause very poor central vision, but this is commoner in the 'wet types'. If your conditions is severe wet (example) scarring is likely. See a scar , another. another large |
 |
ARMD and risks for the other eye |
Unfortunately age related macular degeneration can affect
the other eye. See healthy lifestyle above:
this may help. If you do notice a change in your sight, see distortion above. See
a search . Risk
from drusen.
Concerning neovascular or wet type ARMD....
|
|
Rip / tear |
|
Sometimes the retina in the macula area can tear and shrink. This is call a 'rip' or a 'tear' of the pigment epithelium. It may occur spontaneously as part of wet ARMD, but can occur after PDT or anti-VEGF treatment. A rip causes significant loss of central vision. See a case, with reports a pigment epithelial rip (thanks to Ajith Kumar/BMEC). Even the new drugs can cause the retina to 'rip', but the risks are only slightly increased. The chances of rip depend on how elevated the PED is (the retinal pigment epithelial detachment). For instance, an 840μ elevation has a 50% chance of ripping. A 500μ elevation has a 10% chance of ripping. Gelsiken 2009 |
Rip: separate page for printing.
|
Abbreviations |
|
Here is a summary of some of the abbreviations ophthalmologists use in this condition: |
| CNV | choroidal new vessels (i.e. neovascular
macular degeneration, or 'wet'). Blood vesssels growing through the retina
under the macula. Also called CCNV. |
| CNVM or CNVm | a choroidal neovascular membrane, that is a network of CNV, although in practice this means the same thing as CNV |
| ARM | age-related macular disease |
| ARMD | age-related macular degeneration |
| PDT | photodynamic therapy (for classic sub-foveal neovascular ARMD ) |
| Occult CNV | hard-to-see neovascular ARMD (based
on angiogram) blood vessels growing under the retina and leaking (but the leakage is late) |
| Classic CNV | easy-to-see neovascular ARMD (based on angiogram) blood vessels growing under the retina and leaking |
| dry ARMD | thinning (and other changes) of the central retina |
| PED | pigment epithelial detachment, a type of wet ARMD |
| Rip | a pigment epithelial rip or tear |
| VEGF | Vascular endothelial growth factor...the main chemical that makes blood vessels grow in ARMD |
| RAP | retinal angiomatous proliferation |
| OCT / scans | optitcal coherence tomogram: a 3 dimensional photograph of the macula, called a scan |
| VMC | Virtaul macular clinic..patients attend for an OCT and the scan is interpreted later, and the patient contact if another anti-vegf injection is needed |
| wet (armd) | wet age-related macular degeneration, with CNV as above (blood vessels growing and leaking under the retina, usually under the macula) |
| neovasularisation | similar meaing to wet armd |
| macula | the centre of the retina that sees detailed vision like faces and reading |
| anti-VEGF / injection | drugs that reduce growth and leaking from the new blood vessels under the retina in arnd, or on the retina in diabetes etc. They are gvine by injection into the eye |
| GP | general pratitioner |
| drusen | a type of aging change of the retina...tiny white spots/areas |
Links |
| some facts, USA, |
http://www.nei.nih.gov/health/maculardegen/armd_facts.asp |
| support, USA | Macula Degeneration Support Website |
| animation | http://www.eyesight.org/Macular_Degeneration/Pictorials/pictorials.html |
| anatomy | http://webvision.med.utah.edu/book/part-ii-anatomy-and-physiology-of-the-retina/ |
| more facts, UK | Royal National Institute for the Blind |
| support, UK |
http://www.maculardisease.org [email protected] ARMD web site http://www.armd.org.uk/index.html |
| photos | Some useful photos http://eyephoto.ophth.wisc.edu/. |
| depression | this is common and can be prevented/treated See our LVA page |
|
thanks to |
Photos thanks to Good Hope and BMEC photographers/staff |
�
| The address of this site ('org' changing to 'nhs') is changing from http://www.goodhope.org.uk/departments/eyedept/ to http://www.goodhope.nhs.uk/departments/eyedept/ |
|