Glaucoma (adults) & chronic open angle glaucoma David Kinshuck |
|
|
Introduction |
|
Glaucoma is usually caused by too much fluid pressing on the nerve at the back of the eye. There are many types of glaucoma, but on this page glaucoma is the term given to the 'chronic open angle' or 'primary open angle' or 'chronic simple' glaucoma. Pseudoexfoliation and pigmentary glaucomas are both chronic open angle glaucomas, and this page applies. Glaucoma is not a single disease, but represents conditions that occur for different reasons with the final event being optic nerve damage and visual field loss (Caprioli). |
Types of glaucoma
|
Parts of the eye involved |
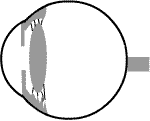 |
|||||
| The eye is a round ball the size of a small tomato. | |||||
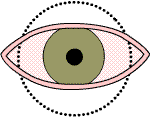 |
It is partly hidden behind the eyelids. | ||||
 |
Imagine the eye turning as shown below... | ||||
 |
|||||
turning
more.. |
 |
||||
 |
||||
then
imagine 'cutting' through the eye ball... |
||||
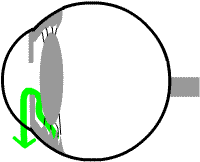 |
||||
.....this is the view used below to explain glaucoma. The green arrow shows the flow of fluid, like water, through the eye. |
||||
The optic nerve in glaucoma |
|
The optic nerve is the 'electric wire' of the eye, an it takes messages about what you see on towards the brain. In the main type of glaucoma the optic nerve is pressed on by extra fluid in the eye, and this may damage the sight in the eye. See photos |
|
How does glaucoma develop? |
|
Everybody's eye produces a fluid like water in its middle chamber.
This fluid then flows around inside the eye to the front chamber,
as shown in the diagram below... the blue arrow. Then, from the front chamber the fluid leaves the eye by entering a drainage meshwork, like the drainpipe of a sink or bath. From this drainage system the fluid enters the bloodstream. The trabecular meshwork is a type of filter system. In the common type of glaucoma this drainage system can block. The
fluid gets trapped in the eye, and the pressure inside the eye goes
up like a tyre being blown up to much. The pressure reduces the blood flow in the tiny blood vessels in the optic nerve. Intraocular presure is strongly related to the metabolic syndrome (Nature 2010) "Metabolic syndrome and other insulin resistance-related features, including hepatic steatosis, increased left ventricular mass, and proteinuria, are strongly associated with IOP". |
Normally fluid is made in the ciliary body and circulates to the front chamber, where it drains through the trabecular meshwork out of the eye. enlarge
|
|
|
The eye produces its own fluid, like a 'tap in the bathroom', in its middle chamber. The fluid ...like water.. flows through from the middle to the front chamber, the eye. The fluid then drains out of the eye through a 'drain' , like the plughole of a sink (the trabecular meshwork). If the drain blocks, the fluid cannot get out of the eye, and the pressure in the eye builds up like a car tyre being pumped up too much. This pressure damages the optic nerve at the back of the eye, pressing it in (lower diagram). enlarge |
Use your mouse to identify parts of the eye; aqueous flow |
|
|
Blood flow to your optic nerve in glaucoma |
Content on this page requires a newer version of Adobe Flash Player.
|
Genes and your relations |
|
Glaucoma is much commoner as we get older but tends to run in families.
Genes control the blockage of the drain (the 'trabecular meshwork'). The relations of patients with glaucoma should all be checked for the condition. If you have glaucoma and you are 70y, then all the relations (mainly children and sisters and brothers) should be checked from the age of 50y. If you have glaucoma age 30y, then even the children related to you should be checked (again: sons/daughters/brothers/sisters). See. There are 3 particular genes (open angle glaucoma), as decribed Eye 2011. Myocillin group.These influence the drainage of aqueous humour through the trabecular meshwork. For instance, and abnormal protein may be produced, and this becomes trapped in the trabecular meshwork cells, and is toxic. Optineurin groupThese influence the axons in the optic nerve in low tension glaucoma. The retinal ganglion cells are weaker than usual and die earlier. Other genesThere are many other genes: some affect the optic nerve, others affect the trabecular meshwork cells (transport across membranes. Others are related to blood fat levels (toxic to the optic nerve). MyopiaThere be be visual field defects that may be glaucoma related AJO 2011
|
The sight in glaucoma |
|
At first the sight is normal, but it if the glaucoma
is severe, the sight may get progressively worse as opposite. |
 At first the sight is normal,
then a small area of poor vision may develop.
or nearly all the sight.
A common type of loss of vision in glaucoma. |
How does the doctor or optometrist know you have glaucoma? |
Glaucoma is found by an ophthalmologist or optometrist by
|
Treatment for chronic glaucoma in adults |
Chronic glaucoma is treated with |
|
| Drops |
Drops are described in more detail. In practice the maximum combination of drops that can be used
with few side effects are these 3 drops combined, such as xalatan
at night, timolol LA morning, and azopt 2-3 times a day. |
| Laser | Laser may help a little in older patients, see. Argon laser trabeculoplasty is the main operation available, but selective laser trabeculopasty may be more effective. |
| Surgery | However, it is occasionally necessary, especially for younger patients and patients with advanced glaucoma. See some notes here. See animation. Here are Good Hope mitomycin results. Some wonderful videos and other information here. Some patients, especially older patients or those who have had previous trabeculectomy, may need cyclodiode laser. |
Will the sight get worse? |
| Once the pressure reaches a satisfactory level the glaucoma should not
A satisfactory pressure if the optic nerve is healthy is 18-20mmHg, if the nerve is slightly damaged 14-16, and if considerably damaged 10-12 would be ideal. (The pressure level needed also depends on your type of glaucoma. People with 'low tension glaucoma' need a lower pressure, for instance.) People who have a pressure of 14 that never rises above 14 usually notice little progression. Effectively research has shown that if a pressure is 10mmHg, hardly any eye will be further damaged from pressure, if 11mmHg, then 10% of eyes/patients will notice a deterioration, and so on up to 20mmHg. It is very hard for an ophthalmologist to tell which eyes will get worse, but
At 20mmHg most eyes will deteriorate. But in practice the
risks of treatment, such as having to use lots of drops,
and particularly that of diamox tablets or surgery, have
to be balanced against the ideal of seeking a pressure of
10 for all patients. In practice accepting a higher pressure
in a particular patient may still mean very few patients
notice much deterioration, and is the best option. Indeed,
in an elderly patient using 2 or 3 drops there may be no
safe alternative, especially if this includes xalatan (or
lumigan or travaprost). |
Tests each visit |
At each visit these results will be analysed
|
OCT scans |
New equipment can help make the diagnosis, but such tests are often inconclusive. This scan shows 'suspicious' discs, the patient may have glaucoma ('glaucoma suspect': visual fields were full and pressures normal). Glacuoma is more likely to be present if the comp[uter measures a thinnner nerve fibre layers, as indicated in red (the circles surrounding the optic disc, white arrow, 0.7 cupping right and left).
|
Your general health in glaucoma/intraocular hypertension |
|
Remember that your general health and lifestyle have a major impact on glaucoma and your sight. BJO 12
|
| The address of this site ('org' changing to 'nhs') is changing from http://www.goodhope.org.uk/departments/eyedept/ to http://www.goodhope.nhs.uk/departments/eyedept/ |
|